Patients don’t pay for appointments. They pay for outcomes and experiences they trust. In group practices, personalized patient care compounds value by aligning providers, systems, and patient expectations into one consistent journey.
That shift, such as appointments to outcomes, is redefining how successful group practices operate today. As practices grow, add providers, and serve larger patient populations, care often becomes standardized for efficiency.
While standardization improves output, it can unintentionally dilute the patient experience. The result? Patients feel processed instead of cared for.
Personalized patient care changes this equation. In a group practice context, personalization isn’t about individual providers “trying harder.” It’s about designing systems that deliver relevant, consistent, patient-centered experiences, no matter which clinician a patient sees.
By integrating healthcare IT solutions, practices can streamline workflows and ensure critical patient information is always accessible, improving the overall care journey.
This is why personalized care is no longer a “nice to have.” It’s strategically essential. It improves outcomes, increases retention, reduces operational friction, and strengthens trust at scale.
The future of group practice success lies in moving from traditional, reactive care models to proactive, personalized ones, built intentionally into workflows, technology, and team culture.
Using healthcare automation solutions helps automate routine administrative tasks while preserving a human-centered approach, allowing providers to focus on delivering meaningful patient interactions.
What Is Personalized Patient Care?
Personalized patient care differs from standard, one-size-fits-all approaches. While traditional care often follows hard protocols and generalized schedules, personalized approaches adapt to the unique needs, preferences, and health histories of each patient.
Clinical personalization may include customized treatment plans, individualized care delivery, or patient-specific care recommendations.
Non-clinical personalization can cover communication preferences, appointment scheduling, follow-ups, and even how educational materials are delivered. Together, these touchpoints ensure that patients feel heard, understood, and valued at every step.
Implementing patient flow solutions can further enhance personalization by optimizing how patients move through the clinic, reducing wait times, and ensuring each interaction is meaningful.
Patient expectations are central. Today’s patients increasingly seek experiences that are not just efficient but meaningful. Perception matters: when patients feel their care is tailored to them, trust and engagement rise naturally.
For instance, a patient with diabetes may benefit not only from a tailored medication plan but also from personalized reminders about nutrition and exercise, access to educational content relevant to their condition, and scheduled follow-ups that fit their lifestyle. This comprehensive approach turns routine appointments into meaningful interventions.
Why Personalized Care Matters in Group Practices
For group practices, investing in personalized care models offers multiple advantages, both clinical and operational.
Stronger Patient Engagement & Satisfaction

When patients receive care that feels relevant and individualized, engagement improves. Personalized communication, whether through SMS reminders, email updates, or app notifications, helps patients stay informed and involved in their treatment journey.
Consider a patient recovering from surgery. Receiving a personalized care plan, including follow-up instructions, exercise recommendations, and diet tips through their preferred communication channel, makes the patient feel supported beyond the clinic walls. This heightened engagement translates into satisfaction, loyalty, and a willingness to follow through with care recommendations.
Better Clinical Outcomes
Customized treatment plans and patient-specific care can reduce complications and improve adherence. When care aligns with a patient’s health goals, lifestyle, and preferences, recovery times shorten, and outcomes improve.
For example, a patient with hypertension who receives a treatment plan adjusted for their diet, work schedule, and stress levels is more likely to take medications correctly and monitor their blood pressure regularly.
Data-driven personalization ensures that interventions are proactive rather than reactive, preventing complications before they arise.
Increased Patient Trust and Loyalty
Trust grows when patients feel that their care is coordinated and attentive, regardless of which clinician they see. Care personalization in healthcare fosters consistency, reduces anxiety, and strengthens the patient-provider relationship. Loyal patients are more likely to stay with a practice, refer others, and actively participate in their own care.
A study from the Journal of Medical Practice Management found that patients who experienced coordinated and personalized care were 25% more likely to continue treatment with the same practice and recommend it to friends or family.
Higher Patient Retention & Reduced Churn
A patient-centered approach reduces cancellations and no-shows while increasing long-term retention. By making the patient experience seamless and meaningful, group practices can achieve sustainable growth without relying solely on marketing or external referrals.
For instance, sending customized appointment reminders and follow-ups based on a patient’s history and preferred communication method has been shown to reduce no-show rates by up to 30% in multi-provider practices.
What Do Today’s Patients Really Expect?
Modern patients have high expectations. Research shows that patients value responsiveness, clarity, and inclusion in decision-making. They want communication that fits their lifestyle, understandable explanations of treatment options, and the ability to participate in their own care journey.
Patients consistently report that personalized attention makes a tangible difference in their experience. One survey found that patients are more likely to trust and follow advice when communication is tailored to their needs, and treatment plans consider their personal goals. Emotional satisfaction, feeling valued, respected, and heard, directly corresponds with compliance and loyalty.
Patients increasingly expect digital interactions to match their preferences. For example, some prefer app-based notifications for test results, while others want direct phone communication.
Tools like an AI medical receptionist can help practices meet these expectations by managing appointments, reminders, and patient inquiries in real time, ensuring communication is timely, personalized, and efficient. Recognizing these differences and acting on them is a hallmark of patient care customization.
Elements of Personalized Patient Care

Creating tailored patient care involves several key elements.
1. Personalized Communication
Timing, tone, and channel choice are crucial. Some patients prefer SMS reminders, while others may rely on email or app notifications. Messaging should reflect a patient’s conditions, history, and preferences. Personalized communication also includes transparency about care plans, follow-up schedules, and test results.
Example: A patient with asthma might receive reminders to refill medications ahead of seasonal changes, along with tips on managing triggers, while a patient with arthritis might get physical therapy reminders tailored to their mobility goals.
2. Tailored Care Plans
Individualized care delivery ensures that treatment aligns with each patient’s unique needs. Chronic disease management requires different attention than acute care. Lifestyle, personal goals, and existing health conditions should inform every plan, creating a roadmap that patients can follow confidently.
In a group practice, this might mean coordinating between multiple providers so that a patient sees a consistent, integrated care plan rather than fragmented advice. Care coordination ensures that all providers work from the same patient-centered framework.
3. Data-Driven Personalization
Leveraging patient health records and analytics allows practices to identify care gaps and anticipate needs. Predictive insights from EHR systems enable providers to deliver proactive recommendations, improving outcomes while minimizing unnecessary interventions.
For instance, analytics might flag a patient at risk for diabetes complications, prompting early education, diet interventions, or additional monitoring. This proactive approach is at the heart of personalized care models.
4. Patient Education & Shared Decision-Making
Patients are more engaged when they understand their treatment options. Providing customized educational resources, risk calculators, and visual care plans empowers patients to participate actively in decisions about their health. Shared decision-making builds trust, fosters adherence, and reinforces the value of patient-centered care.
Imagine a patient with heart disease using an interactive app to understand the risks of different treatment paths. When the patient collaborates in choosing a plan, adherence and satisfaction increase significantly.
How Group Practices Deliver Personalized Care
Implementing personalized care models requires intentional design in both technology and workflow.
- Team Huddles & Coordinated Workflows: Regular collaboration ensures that all providers are aligned and aware of patient-specific needs.
- Personalized Scheduling & Reminders: Schedules account for patient preferences and treatment priorities.
- Follow-up Protocols Tailored to Patient Journeys: Automated reminders, check-ins, and follow-up messages reinforce care plans.
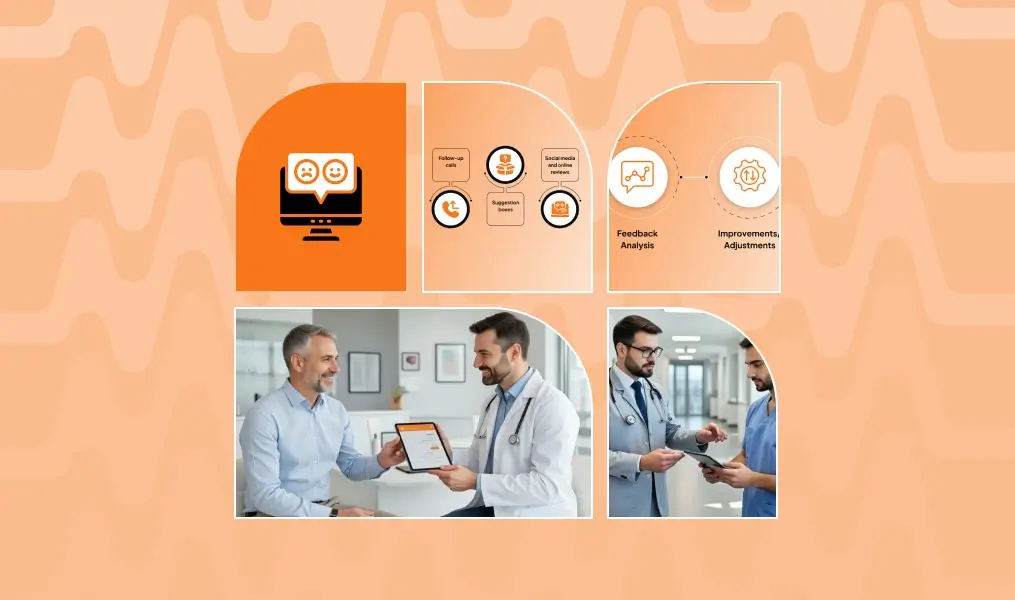
- Feedback-Driven Adjustments: Surveys and experience data help refine communication, workflow, and clinical interventions.
By embedding personalization into these operational mechanisms, group practices can maintain high-quality care at scale.
Benefits of Personalized Care for Group Practices
1. Better Clinical Outcomes
- Improved adherence to treatment plans
- Fewer complications
- Faster recovery times
By focusing on patient-specific care, practices can proactively address risks and monitor progress. Additionally, practices can reduce unnecessary tests or procedures by using predictive insights, improving both outcomes and patient satisfaction.
2. Stronger Patient Loyalty
- Reduced cancellations and no-shows
- Increased referrals from satisfied patients
- Higher long-term retention
Patients are more likely to recommend a practice that values their individual needs and consistently delivers personalized treatment care. Loyalty also translates into long-term engagement, which is critical as healthcare increasingly moves toward value-based care.
3. Improved Operational Efficiency
- Less reactive care, fewer emergency interventions
- Optimized resource allocation
- Reduced burden on front desk and clinicians
A well-structured care personalization in healthcare framework streamlines workflows, allowing staff to focus on value-driven tasks instead of administrative fire-fighting. It also allows practices to scale effectively without compromising the patient experience.
How to Start Implementing Personalized Care
Group practices can take the following actionable steps:
- Audit Current Patient Experience: Identify gaps in communication, treatment plans, and follow-ups.
- Define Personalization Goals: Clarify what “personalized care” means for your practice and patients.
- Choose the Right Tools: Invest in EHRs, patient engagement platforms, and analytics that support individualized care delivery.
- Train Staff: Educate clinicians and administrative teams on delivering consistent, patient-centered experiences.
- Collect Feedback Loop: Use surveys and experience data to assess satisfaction and identify areas for improvement.
- Measure and Refine: Continuously evaluate outcomes, engagement, and retention to ensure patient care customization remains effective.
Future of Personalized Care in Group Practices
The next frontier of personalized patient care will integrate advanced technologies:
- Predictive Analytics: Anticipating care needs before complications arise.
- AI-Driven Patient Insights: Using machine learning to tailor recommendations and communication.
- Genomic and Precision Medicine: Treatments informed by individual genetics and biomarkers.
- Voice/Text AI for Communication: Streamlined patient engagement through conversational interfaces.
These innovations will make healthcare personalization more precise, efficient, and scalable, allowing group practices to deliver experiences once only possible in boutique or private care settings.
Conclusion
Personalized patient care is no longer optional; it is a strategic imperative for group practices seeking sustainable growth. By focusing on patient-centered care, customized treatment plans, and coordinated workflows, practices can improve outcomes, enhance loyalty, and streamline operations simultaneously.
The opportunity is clear: practices that embrace personalization today will not only meet patient expectations, but they will exceed them, setting a new standard for quality, efficiency, and trust in healthcare.
FAQs
What is personalized patient care?
It’s care designed around each patient’s unique needs, preferences, and health history, combining clinical and non-clinical personalization.
How does personalized care affect patient outcomes?
Personalization improves adherence, reduces complications, and enhances overall satisfaction and trust.
What technology supports personalized care?
EHRs, patient engagement platforms, analytics tools, and AI-driven communication systems are key enablers.
How do you measure personalization success?
Metrics include patient engagement, satisfaction scores, retention rates, adherence, and clinical outcomes.
What are common barriers to personalization?
Barriers include fragmented systems, limited staff training, inconsistent workflows, and under-utilization of technology.