Have you ever noticed why some patients leave frustrated, while others are satisfied, after visiting the same doctor? The waiting room of your clinic tells a story to each patient about your clinic’s operations, but are you listening?
The biggest patient flow issues in GP (Group Practice) clinics aren’t where most people expect them to be. Many of these challenges are embedded in everyday workflows and have become so routine that they often go unnoticed.
The organized patient flow in GP clinics is important for providing timely and better care quality and maintaining patient satisfaction, especially when supported by modern healthcare IT solutions. Though several clinics may struggle with problems and incompetence that impact both staff and patients.
So, here in this blog, you’ll find the top 10 patient flow issues and the root causes in GP clinics.
Table of Contents
What is Patient Flow in Group Practice Clinics?
Patient flow in GP clinics means how smoothly patients go through a clinic visit, from the time they arrive until they leave.
On the other hand, poor patient flow leads to patient frustration, longer waits, and staff stress, ultimately resulting in poorer health outcomes.
One study found average wait times of 41 minutes from registration to consultation, with longer waits linked to lower patient satisfaction.
When patient flow runs smoothly, patients wait less and get more care, staff can stay organized, and the clinic runs more efficiently. Studies also show that long waits often increase frustration for both patients and staff.
The 10 Most Common Patient Flow Problems in GP Clinics
Below are the most common challenges faced in healthcare, including long waits and inefficiencies. Patient flow management solutions can help address these issues and streamline clinic operations.
1: Long Wait Before Consultation

Patients often face long waits before seeing a clinician. These delays can happen in the waiting room or between the consultation and discharge. As a result, patients may feel frustrated, dissatisfied, and view the care as inefficient.
Root Causes:
- Appointment schedules often don’t match patients’ actual needs. Some visits take longer than expected, while others are shorter, but fixed time slots treat every appointment the same. This can cause delays and make patients wait longer than necessary.
- Clinics often overbook appointments to make up for missed visits. This can overwhelm staff and make wait times longer for everyone.
- Unpredictable events like late arrivals, longer consultations, or sudden clinical needs can disrupt the schedule. These delays can build up and affect later appointments.
2: Inefficient Scheduling Systems
Inefficient scheduling systems can cause backlogs and idle periods, which disrupt the steady movement of patients through the clinic. These problems frustrate patients, add stress for staff, lower productivity, and may reduce the quality of care.
Root Causes:
- When self-service online booking is limited, patients have to rely on phone calls or talking to front desk staff to make appointments. This adds to the administrative workload and can delay getting timely appointments.
- There is often a mismatch between patient demand and available appointment slots, especially during busy times. This can cause overbooking, long waits, and empty slots during slower periods. These issues disrupt patient flow and reduce clinic operational efficiency.
3: Staff Shortages and Burnout
Clinics facing staff shortages often struggle to keep patient flow smooth, leading to delays at multiple points, including check-in, rooming, and the consultation itself. These interruptions not only affect the patient experience but also place significant pressure on existing staff, creating a cycle of stress, inefficiency, and dissatisfaction.
Root Causes:
- Staff members are frequently overburdened, balancing clinical responsibilities with administrative tasks such as scheduling, documentation, and patient coordination, which reduces their capacity to manage patient flow efficiently.
- Chaotic workflows and constant pressure contribute to high levels of stress, fatigue, and burnout among healthcare workers. This can lead to higher staff turnover, making staffing shortages worse and disrupting continuity of care.
4: Manual Administrative Processes

Using paper-based or manual administrative processes can slow key clinic tasks such as patient check-in, documentation, billing, and discharge. These delays make patients wait longer, increase the chance of mistakes, and lower overall efficiency.
Root Causes:
- Many clinics still use manual forms and registration, so staff have to enter data by hand. This takes a lot of time and can lead to mistakes.
- When medical records, insurance checks, and other admin tasks are not managed well, problems can happen. This is especially true during busy times or with complicated cases.
- Without digital workflows and automation, staff spend too much time on repetitive tasks. This raises the risk of errors, slows down patient flow, and makes the clinic less efficient.
5: Poor Communication and Coordination
When clinic staff fail to communicate or coordinate effectively, patient care can be delayed, and problems may arise at multiple points throughout the patient journey.
Poor communication not only slows down work but also increases the risk of errors, creates duplicated tasks, and negatively impacts the overall patient experience, contributing to significant patient flow inefficiencies.
Root Causes:
- Disconnected systems and the lack of real-time information sharing make it challenging for staff to access accurate patient data when needed, leading to delays in care and slower decision-making.
- Inefficient handoffs between the front desk, clinical staff, and billing teams can create confusion and prolong essential tasks, such as rooming patients, updating medical records, or processing payments.
- Unclear roles, responsibilities, and workflows increase the likelihood of duplicated work, miscommunication, and reduced operational efficiency, all of which disrupt the smooth movement of patients through the clinic.
6: Clinic Layout and Physical Restrictions

A poor clinic layout can significantly delay the smooth movement of patients and staff, creating unnecessary delays and limiting access to essential services.
Inefficient use of space can lead to congestion, confusion, and a sub-optimal patient experience, ultimately reducing clinic operational efficiency.
Root Causes:
- Patients and staff often have to backtrack or navigate awkward pathways due to poorly designed spaces, which slows down transitions between check-in, consultation, and discharge areas.
- Examination rooms may not be standardized in terms of size, equipment placement, or setup, making it difficult for clinicians to move quickly between patients and for staff to support clinical workflows efficiently.
- Essential medical equipment and supplies may be poorly located or inconsistently placed, forcing staff to spend extra time searching or moving items, further contributing to patient flow delays.
7: Walk-In and Unscheduled Visits
Unplanned walk-in or unscheduled visits can disrupt the day’s carefully planned schedule, causing delays not only for the arriving patients but also for those with pre-booked appointments.
These interruptions can slow down overall clinic operations, create congestion in waiting areas, and increase stress for staff, ultimately impacting patient satisfaction and care quality.
Root Causes:
- Many clinics lack dedicated slots or effective strategies to accommodate walk-in patients without destabilizing the existing schedule, which leads to unexpected interruptions and patient flow delays.
- When clinics avoid flexible scheduling, unscheduled visits can disrupt the day, leading to longer waits and slower operations.
- Without a clear system for handling walk-ins, front desk and clinical staff must constantly reprioritize tasks, which slows down patient processing and creates a ripple effect that impacts the entire day’s workflow.
8: No-Shows and Late Arrivals
Missed appointments and late arrivals can significantly disrupt a clinic’s daily schedule, leading to inefficient use of time and resources.
When patients do not arrive as planned or show up late, it not only affects their own care but also creates delays for other patients, extend staff workloads, and reduce overall clinic productivity.
Root Causes:
- Many clinics lack effective reminder systems or confirmation mechanisms, such as automated calls, texts, or emails, that help ensure patient recall and adherence to scheduled appointments.
- Some clinics don’t have clear policies to manage late arrivals, leaving staff to handle disruptions as they come, which causes frustration and inconsistency.
- Scheduling systems are often not designed to absorb variability, such as late arrivals or no-shows, which makes it difficult for clinics to adjust in real-time without creating delays for other patients.
9: Billing and Discharge Delays

Even after a consultation is complete, delays in billing, follow-up scheduling, and patient education can significantly slow down patient discharge.
These delays not only prolong the patient’s time in the clinic but also create issues that affect subsequent appointments, staff workload, and overall operational efficiency.
Root Causes:
- Reliance on manual billing processes and insurance verification procedures consumes considerable staff time, often leading to errors and slower processing of patient accounts.
- A lack of integrated discharge planning and follow-up coordination means that patients may leave without clear instructions or next steps, requiring additional staff intervention and further extending their stay.
- Inefficient handoffs between clinical and administrative staff can result in miscommunication, duplicated efforts, and delays in completing necessary discharge tasks, all of which contribute to slower patient throughput and operational inefficiencies.
10: Inefficient Patient Management in Busy Hours
When clinics are not well-organized during busy hours, patients often experience long waits and confusion. Delays and disorganization can make patients feel ignored or frustrated, leading to lower satisfaction and loss of trust in the clinic.
Poor management during peak times also affects the clinic’s reputation and can make patients less likely to return.
Root Causes:
- Long waiting times and slow handling of patients leave them feeling unimportant.
- Staff may not communicate clearly, or consultations may feel rushed, reducing confidence in care.
- Patients’ needs may not be fully met, such as delays in getting prescriptions, limited time with the doctor, or unclear instructions for follow-up.
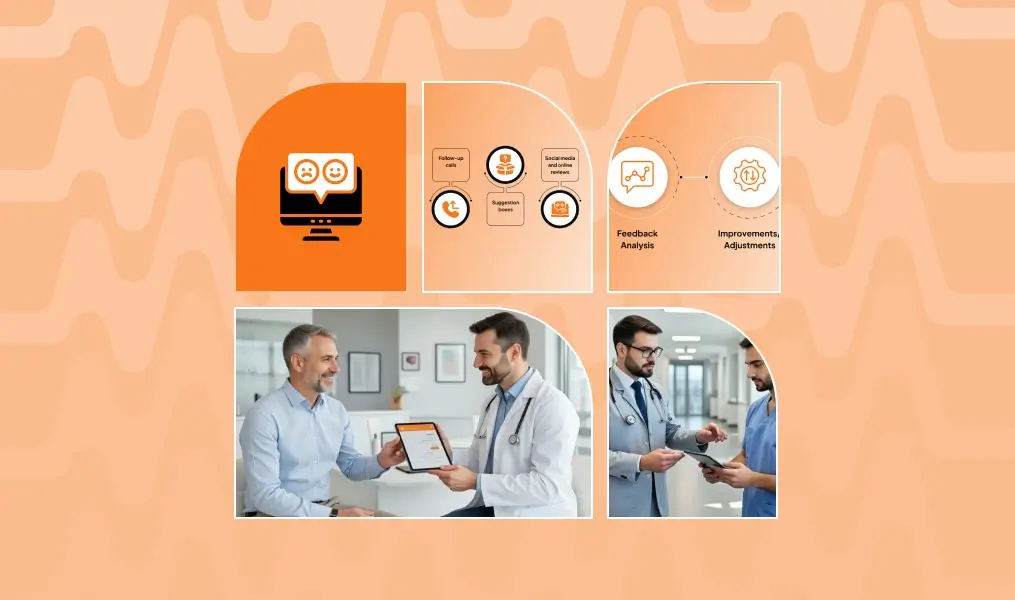
Conclusion
Efficient patient flow is essential for delivering high-quality care in GP clinics. Long waits, inefficient scheduling, staff shortages, manual administrative processes, poor communication, and suboptimal clinic layouts not only slow operations but also affect patient satisfaction, staff well-being, and overall clinic performance.
Patients notice delays, and repeated frustrations can erode trust, lower retention, and generate negative feedback. Overworked staff face stress and reduced productivity, further impacting the patient experience.
Understanding and addressing these issues is the first step toward improvement. Optimizing appointment management, digital check-ins, internal communication, and clinic design can create a smoother, more organized patient journey.
MedLaunch provides a comprehensive solution to tackle these inefficiencies. Our AI-powered solutions manages every stage of the patient experience, including scheduling, check-in, consultation, discharge, and follow-up.
Improving patient flow is no longer optional, it is essential for better care, happier patients, and a more productive clinic. Let MedLaunch transform your operations and create a seamless experience for everyone.
FAQs
How can GP clinics identify patient flow problems early?
Clinics can monitor wait times, appointment delays, and staff workload regularly. Early tracking helps spot inefficiencies before they affect patients or staff.
How does patient flow differ between peak and off-peak hours?
During peak hours, clinics experience longer waits and higher staff stress. Off-peak hours are generally smoother, with faster patient movement and less pressure on staff.
How does patient flow affect clinic revenue?
Inefficient patient flow reduces the number of patients seen and increases idle time. This directly lowers revenue and clinic productivity.
How does patient flow impact patient trust and satisfaction?
Smooth patient flow makes patients feel valued and well-cared-for. Delays or disorganization can frustrate patients and reduce their trust in the clinic.
Can improving patient flow reduce staff turnover?
Efficient workflows reduce stress, fatigue, and burnout among staff. Happier, less-stressed employees are more likely to stay, lowering turnover rates.